Fibrillazione ventricolare
Revisione paritaria di Dr Toni Hazell, MRCGPUltimo aggiornamento di Dr Hayley Willacy, FRCGP Ultimo aggiornamento 23 May 2023
Rispetta le linee guida editoriali
- ScaricaScarica
- Condividi
- Language
- Discussione
Professionisti Medici
Gli articoli di riferimento professionale sono progettati per essere utilizzati dai professionisti della salute. Sono scritti da medici del Regno Unito e basati su prove di ricerca, linee guida del Regno Unito e europee. Potresti trovare il Abnormal heart rhythms articolo più utile, o uno dei nostri altri articoli sulla salute.
In questo articolo:
What is ventricular fibrillation?
Ventricular fibrillation (VF) is a cause of cardiac arrest and sudden cardiac death. The ventricular muscle fibres contract randomly causing a complete failure of ventricular function. Most cases of ventricular fibrillation occur in patients with pre-existing known heart disease (with myocardial fibrosis - scarring - having a role1 ) but the precise nature of the underlying cause of VF is not currently known.
How common is ventricular fibrillation? (Epidemiology)
Torna ai contenutiVF is the most commonly identified arrhythmia in cardiac arrest patients and has been reported as present in 70% of cardiac arrests.2
The incidence of VF parallels the incidence of ischaemic heart disease, with a peak incidence of VF occurring in people aged 45-75 years.
Fattori di rischio
VF is most often associated with coronary artery disease and as a terminal event. VF may be due to acute myocardial infarction (MI) or ischaemia, or occur because of a chronic infarction scar.
When electrocardiogram documentation is available, it often shows that rapid VT precedes VF.
VF can occur during any of the following conditions or situations:
Antiarrhythmic drug administration.
Ipossia.
Ischaemia.
Very rapid ventricular rates in the pre-excitation syndrome.
Electrical shock administered during cardioversion.
Electrical shock caused by accidental contact with improperly grounded equipment.
Competitive ventricular pacing to terminate ventricular tachycardia (VT).
VF can occur in healthy, young athletes after a blunt (non-penetrating) blow to the chest.3 This known as commotio cordis.
Continua a leggere sotto
Presentation of ventricular fibrillation
Torna ai contenutiPatients may have a history of chest pain, fatigue, palpitations and other nonspecific complaints.
There may be known diagnosis or suggestion of pre-existing heart disease - eg, coronary artery disease, cardiomyopathy, valvular heart disease, miocardite, congenital heart disease, long QT syndrome, Wolff-Parkinson-White (WPW) syndrome or Brugada's syndrome.
Diagnosi differenziale
Torna ai contenutiArrhythmias associated with cardiac arrest are divided into two groups:
Shockable rhythms: VF and VT.
Non-shockable rhythms: asystole and pulseless electrical activity (PEA): see the separate article on Adult Cardiopulmonary Arrest.
Other causes of sudden collapse such as aortic dissection e embolia polmonare.
Continua a leggere sotto
Indagini
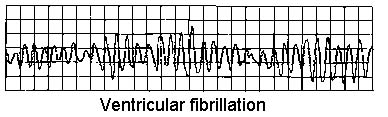
Torna ai contenutiVENTRICULAR FIBRILLATION
Cardiac enzymes (troponin).
Electrolytes, calcium and magnesium. Severe metabolic acidosis, hypokalaemia, hyperkalaemia, hypocalcaemia, and hypomagnesaemia are some of the conditions that can increase the risk for arrhythmia and sudden death.
Drug levels (eg, tricyclic antidepressants, digoxin). Most of the anti-arrhythmic medications also have a pro-arrhythmic effect.
Toxicology screen: drugs that can lead to vasospasm-induced ischaemia - eg, cocaine.
Ormone stimolante la tiroide (TSH): hyperthyroidism can lead to tachycardia and tachyarrhythmias.
ECG:4 evidence of MI, prolonged QT interval, short PR, WPW pattern or other conditions.
CXR: signs of left heart failure, pulmonary hypertension.
Echocardiography: underlying structural abnormalities and cardiac dysfunction.
Nuclear imaging techniques:
Resting thallium (Tl) or technetium Tc 99m scintigraphy: assessing myocardial damage after MI.
Exercise nuclear scintigraphy: very sensitive in detecting the presence, extent and location of myocardial ischaemia.
Angiografia coronarica:
Cardiac catheterisation in patients who survive VF, to assess the state of ventricular function and severity and extent of coronary artery disease.
Coronary angiography identifies patients who may benefit from revascularisation by percutaneous coronary intervention (angioplasty) or coronary artery bypass grafting (CABG), and can also help identify coronary artery anomalies and other forms of congenital heart disease.
Management of ventricular fibrillation2
Torna ai contenutiSee the separate articles on Adult Cardiopulmonary Arrest e Defibrillation and Cardioversion. Early defibrillation is essential to improve outcome.
Medical stabilisation
Patients who survive the initial episode of VF require a full evaluation of left ventricular function, myocardial perfusion and electrophysiological stability.
Careful post-resuscitation care is essential to survival because recurrence rates average at about 50%.
Treatment of myocardial ischaemia, heart failure and electrolyte disturbances.
Empirical beta-blockers are often given.
Most survivors of VF should be treated with implantable cardioverter defibrillators (ICDs).5 Transvenous ICDs can be placed with minimal morbidity and mortality.
Radiofrequency ablation: most cases of VF are not amenable to radiofrequency ablation and require ICD placement.
By itself, CABG only prevents recurrent VF if the ejection fraction is normal and ischaemia was the cause of the arrest. Even in these patients, ICDs are frequently placed after CABG.
Complications of ventricular fibrillation
Torna ai contenutiCentral nervous system ischaemic injury.
Myocardial injury.
Post-defibrillation arrhythmias.
Defibrillation injury to self or others.
Injuries from CPR and resuscitation.
Skin burns.
Death.
Prognosi
Torna ai contenutiPrognosis for survivors of VF strongly depends on the time elapsed between onset and medical intervention (prognosis is poor without intervention by 4-6 minutes after onset of VF) as well as on the particular aetiology for the VF.
Early defibrillation often makes the difference between long-term disability and functional recovery.6 If defibrillation is delivered promptly, survival rates as high as 75% have been reported.7
Death and disability after successful resuscitation correlate with the degree of central nervous system damage occurring during the event due to anoxia.
VF that occurs within the first 48 hours of the onset of acute MI has no bearing on prognosis, but VF that occurs more than 48 hours after acute MI is associated with a high rate of recurrence and a poorer prognosis.
After resuscitation, the prognosis is largely dependent on haemodynamic stability, early neurological recovery and duration of the resuscitation.
Education and training of non-healthcare professionals in basic life support and the use of automated external defibrillators in public places probably have the greatest impact on improving survival rates.
A major adverse outcome from a VF event is anoxic encephalopathy.
Ulteriori letture e riferimenti
- Adult Tachycardia Algorithm; Resuscitation Council (UK), 2015 (updated 2021).
- Bezzerides VJ, Pu WT; Two sides of the same coin: new insights into mechanisms of ventricular fibrillation. Cardiovasc Res. 2021 Mar 21;117(4):983-984. doi: 10.1093/cvr/cvaa246.
- Ludhwani D, Goyal A, Jagtap M; Ventricular Fibrillation.
- Patel N, Pena C, Nesheiwat Z, et al; Ventricular fibrillation arrest after blunt chest trauma in a 33-year-old man, commotio cordis? BMC Cardiovasc Disord. 2022 Jun 3;22(1):252. doi: 10.1186/s12872-022-02689-4.
- Biblioteca ECG
- Implantable cardioverter defibrillators and cardiac resynchronisation therapy for arrhythmias and heart failure; NICE Technology Appraisal Guidance, June 2014
- Adgey AA, Spence MS, Walsh SJ; Theory and practice of defibrillation: (2) defibrillation for ventricular fibrillation. Heart. 2005 Jan;91(1):118
- Linee guida 2021 per il supporto vitale avanzato per adulti; Consiglio di Rianimazione UK
Continua a leggere sotto
Storia dell'articolo
Le informazioni su questa pagina sono scritte e revisionate da clinici qualificati.
Next review due: 21 May 2028
23 May 2023 | Ultima versione

Chiedi, condividi, connettiti.
Esplora le discussioni, fai domande e condividi esperienze su centinaia di argomenti di salute.

Non ti senti bene?
Valuta i tuoi sintomi online gratuitamente