Spinal stenosis
Revisione paritaria di Dr Caroline Wiggins, MRCGP Ultimo aggiornamento di Dr Rosalyn Adleman, MRCGPUltimo aggiornamento 24 Jul 2025
Rispetta le linee guida editoriali
- ScaricaScarica
- Condividi
- Language
- Discussione
In questa serie:Back and spine painDolore lombareSlipped discSindrome della cauda equinaThoracic back painMal di schiena nei bambini
Spinal stenosis is a term used to describe a narrowing of your spinal canal. The narrowing may not cause any symptoms. However, the narrowing may progress to cause squeezing (compression) of your spinal nerves or compression of your spine. Spinal stenosis causes back pain and leg pain. Most often it occurs when you walk. Weakness of the legs may make you feel unsteady. This may affect both legs or just one leg. Spinal stenosis affecting the cervical spine in your neck may also cause pain and weakness in the shoulders and arms.
Spinal stenosis can often be treated by simple measures such as medicines for pain relief, keeping as active as you can and losing weight if you are overweight. Sometimes steroid injections or surgery are suggested if simple measures are not successful.
In questo articolo:
Video consigliati per Schiena e colonna vertebrale
What is spinal stenosis?
Spinal stenosis is a term used to describe a narrowing of your spinal canal. The narrowing may not cause any symptoms. However, the narrowing may progress to cause squeezing (compression) of your spinal nerves or compression of your spine. Narrowing that affects your spinal cord is sometimes called a myelopathy. More than one level of your spine may be affected. The blood supply to the nerves in your spine may also be temporarily reduced by the compression.
The lower end of your spinal cord is at the level of the first or second lumbar bone (vertebra). The nerves from your spinal cord then form a structure called the conus medullaris. The spinal nerves continue to branch out below the conus medullaris to form the cauda equina.
Pressure on your cauda equina causes cauda equina syndrome. Cauda equina syndrome may cause low back pain and problems with your bowel and bladder function, numbness in your saddle area, which is around the back passage (anus), and weakness in one or both legs. Cauda equina syndrome needs urgent investigation and treatment to prevent the nerves to your bladder and bowel from becoming permanently damaged.
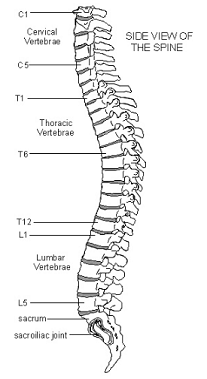
Understanding the back
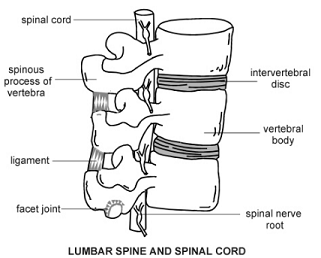
Your spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a disc. The discs are made of strong rubber-like tissue which allows your spine to be fairly flexible. A disc has a stronger fibrous outer part and a softer jelly-like middle part called the nucleus pulposus.
Your spinal cord, which contains the nerves that come from your brain, is protected by your spine. Nerves from your spinal cord come out from between your vertebrae to relay messages to and from various parts of your body.
Spinal cord
Close-up diagram lumbar spinal cord
Spinal stenosis causes
Torna ai contenutiAs you get older, degenerative changes occur in your spine, especially in your lower back and neck. Sometimes this causes partial compression (stenosis) of the nerve tunnel within your spine. This is called central stenosis. Sometimes there is a constriction to the smaller side tunnels within your spine. This is called foraminal stenosis.
Continua a leggere sotto
How common is spinal stenosis?
Torna ai contenutiSpinal stenosis is common, especially in older people. However, it can also rarely affect younger people. Spinal stenosis most often affects your lower (lumbar) spine. The next most commonly affected part of your spine is the cervical spine in your neck. Stenosis of the spine at the back of your chest (thoracic spine) is much less common.
Spinal stenosis symptoms
Torna ai contenutiSymptoms of spinal stenosis include back pain and leg pain. This often occurs when you walk. Weakness of the legs may make you feel unsteady. This may affect both your legs or just one leg. Spinal stenosis affecting your cervical spine may also cause pain and weakness in your shoulders and arms.
Claudication is the term used to describe pain, weakness or numbness of your legs that becomes worse specifically on walking. Claudication is caused either by narrowing of the blood vessels supplying the leg or because of spinal stenosis.
Usually spinal stenosis prevents you from walking beyond a certain distance. You then have to stop because of increasing pain and numbness in one or both of your legs. The symptoms can also occur when standing. Usually the symptoms reduce if you sit down or lean forwards. There is usually no pain when you are resting.
Walking usually only aggravates your leg symptoms. The back pain caused by spinal stenosis does not increase with walking.
Continua a leggere sotto
What tests are used to diagnose spinal stenosis?
Torna ai contenutiIf your doctor thinks that you may have spinal stenosis then an Risonanza magnetica may be needed to confirm the diagnosis.
What is the treatment for spinal stenosis?
Torna ai contenutiHow you can help to improve your own symptoms
Maintain activity as much as you can. Try to gradually increase the distance you walk if you can.
Massage and heat treatments.
Physiotherapy. You may be able to self-refer for this, or your doctor may refer you. There is evidence from scientific trials that manual therapy and exercise is an effective treatment.
Pain relief. Using over-the-counter medication such as paracetamolo o ibuprofene may be sufficient.
Other medicines prescribed by your doctor can be used if over-the-counter medicines do not provide enough pain relief. Some medicines can be used specifically to help the nerve pain in your legs - for example, amitriptilina, gabapentin o pregabalin.
Other available treatments
Spinal injections: injections of a steroid with local anaesthetic given into your spinal root canal or given by epidural injections can be helpful.
Chirurgia: if symptoms still do not improve then one option is surgery. The most commonly used operation is called a decompression. The bone that is compressing the nerves is removed so that the nerves have more room. The two bones (vertebrae) may also be fused together (this is called spinal fusion).
There is very limited evidence for surgery to treat spinal stenosis. The success of surgery for spinal stenosis is variable. Although your symptoms may improve just after the operation, the medium-term and long-term results can be disappointing.
Interspinous distraction: this procedure involves placing an implant between the spinous processes of the affected vertebrae (usually the fourth and fifth lumbar vertebrae) in order to limit you extending your back. This helps to prevent or reduce the pain in your legs when standing or walking.
Qual è il risultato (prognosi)?
Torna ai contenutiThe outcome is variable and, without treatment, the symptoms usually gradually become worse. Although treatments for spinal stenosis are often effective at reducing symptoms, the symptoms don't always completely resolve. Many people can cope with their symptoms, as time can allow the nerves to adapt.
Scelte dei pazienti per Schiena e colonna vertebrale

Ossa, articolazioni e muscoli
Spondiloartrite assiale
Spondiloartrite assiale (nota anche come axSpA o SpA assiale) è un'artrite dolorosa e cronica che colpisce principalmente le articolazioni della colonna vertebrale e anche le articolazioni che collegano ciascun lato della base della colonna vertebrale con il bacino (articolazioni sacroiliache). Può anche colpire altre articolazioni del corpo, così come tendini e legamenti. Si divide in: 1) Spondilite anchilosante. 2) Spondiloartrite assiale non radiografica.
di Dr Philippa Vincent, MRCGP

Ossa, articolazioni e muscoli
Torcicollo
Torticollis significa 'collo storto'. È anche spesso chiamato 'torcicollo'.
di Dr Surangi Mendis, MRCGP
Ulteriori letture e riferimenti
- Interspinous distraction procedures for lumbar spinal stenosis causing neurogenic claudication; NICE Interventional procedure guidance, November 2010
- Zaina F, Tomkins-Lane C, Carragee E, et al; Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Jan 29;(1):CD010264. doi: 10.1002/14651858.CD010264.pub2.
- Kato S, Fehlings M; Degenerative cervical myelopathy. Curr Rev Musculoskelet Med. 2016 Sep;9(3):263-71. doi: 10.1007/s12178-016-9348-5.
- Bagley C, MacAllister M, Dosselman L, et al; Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res. 2019 Jan 31;8. doi: 10.12688/f1000research.16082.1. eCollection 2019.
- Raja A, Hoang S, Patel P, et al; Spinal Stenosis. StatPearls, Jan 2022.
- Ammendolia C, Hofkirchner C, Plener J, Bussières A, Schneider MJ, Young JJ, Furlan AD, Stuber K, Ahmed A, Cancelliere C, Adeboyejo A, Ornelas J. Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. BMJ Open. 2022 Jan 19;12(1):e057724. doi: 10.1136/bmjopen-2021-057724.
Continua a leggere sotto
Storia dell'articolo
Le informazioni su questa pagina sono scritte e revisionate da clinici qualificati.
Next review due: 3 Jul 2028
24 Jul 2025 | Ultima versione
22 Feb 2017 | Pubblicato originariamente
Autore:
Dr Colin Tidy, MRCGP

Chiedi, condividi, connettiti.
Esplora le discussioni, fai domande e condividi esperienze su centinaia di argomenti di salute.

Non ti senti bene?
Valuta i tuoi sintomi online gratuitamente
Iscriviti alla newsletter di Patient
La tua dose settimanale di consigli sulla salute chiari e affidabili - scritti per aiutarti a sentirti informato, sicuro e in controllo.
Abbonandoti accetti il nostro Informativa sulla Privacy. Puoi annullare l'iscrizione in qualsiasi momento. Non vendiamo mai i tuoi dati.